The costs associated with a nosocomial antibiotic-resistant bacterial outbreak can be substantial, but computing the costs is not always straightforward. Financial burden includes both direct and indirect or opportunity costs, such as reallocated staff time, excess or lost bed utilization, or missed revenue for care that would have been delivered in the absence of an outbreak.
The challenge in estimating these costs was demonstrated in a new study out of the United Kingdom where the costs associated with even a modest carbapenemase-producing Enterobacteriaceae outbreak affecting 40 patients during a 10-month period of time had a significant financial impact: €1.1 million ($1.2 million).1 Since outbreaks can result in significant costs, proactive steps, including patient screening with rapid diagnostic tools, could be employed to minimize the impact.
Table 1: Costs Associated With A CRE Outbreak in the United Kingdom
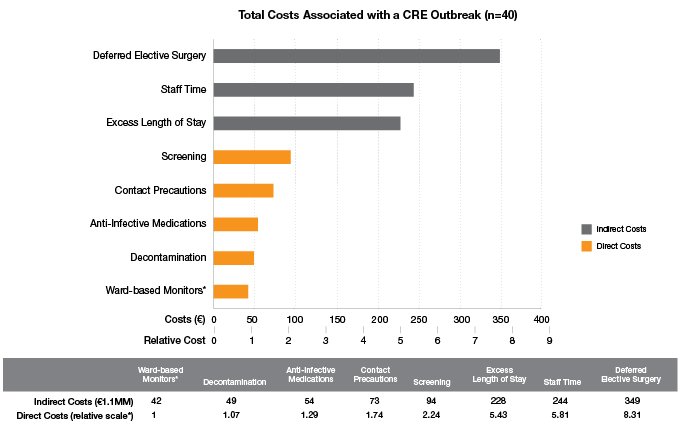
* Relative costs referenced against the least costly parameter, ward-based monitoring
These figures do not take into account costs for facility improvements, legal expenses, the impact on hospital reputation, or the morbidity and mortality associated with an outbreak. Of the 40 patients affected by the outbreak, 16 died, 5 were discharged with end-of-life care plans, 4 required ongoing hemodialysis, 12 required regular outpatient clinic care, and 3 were discharged from the hospital system.
Click here to read the full journal article from Clinical Microbiology and Infection.
1. Otter JA, Burgess P, Davies F, Mookerjee S, et al. Counting the cost of an outbreak of carbapenemase-producing Enterobacteriaceae: an economic evaluation from a hospital perspective. Clin Microbiol Infect. 2016 Oct 13. pii: S1198-743X(16)30464-5 [Epub ahead of print].